As rates of obesity, high blood pressure, type 2 diabetes and sleep apnea increase, cases of advanced chronic liver disease and resulting liver scarring or cirrhosis are also rising. Patients often are diagnosed based on symptoms, such as gastrointestinal bleeding, fluid retention or jaundice, which happen when liver disease has progressed to a late stage. This problem led Mayo Clinic researchers to develop an artificial intelligence (AI) model that resulted in twice the number of advanced chronic liver disease diagnoses in patients without symptoms, helping physicians treat them before the disease had progressed.
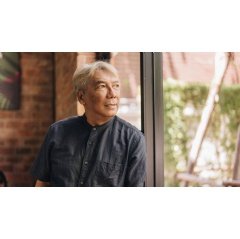
“Chronic liver disease is a progressive condition, so the sooner we can diagnose it, the sooner we can stop it from advancing to irreversible stages. Early intervention may decrease the likelihood that a patient will need a liver transplant in the future,” says Doug Simonetto, M.D., a Mayo Clinic transplant hepatologist and lead author of the study published in Nature Medicine.
The heart and liver are closely linked. Liver scarring may lead to increased local pressure that can affect the heart. As a result, a heartbeat test called an electrocardiogram (ECG) can capture electrical signal changes in the heart connected to advanced liver disease. Dr Simonetto and colleagues developed an AI model to analyse data from 11,513 Mayo Clinic patients undergoing routine ECGs. The model looked for patterns connected to advanced liver disease in the ECG data, and it found twice the number of patients who were diagnosed by standard methods. The diagnosis was confirmed by validated imaging or blood tests.
“As a family physician, I’ve often seen how advanced liver disease — which frequently has no symptoms until it becomes irreversible — can go undetected" says David Rushlow, M.D., Mayo Clinic Health System family physician and study co-author. "Many patients identified through the AI-ECG model had no idea they were living with advanced liver disease. By identifying these cases earlier, we were able to connect them to the right treatment — at a time when intervention can truly make a difference. For these patients, the technology helped us not only to uncover a diagnosis, but it also created an opportunity for better health outcomes and, in some cases, may have saved lives.”